Abstract
Healthcare disparities in Pakistan pose a significant challenge to achieving universal access to quality healthcare services. For a healthcare system to function, proper infrastructure and financial support is required. This policy brief addresses the complexities of healthcare inequalities, highlighting the challenges faced in addressing them and offering innovative and effective solutions. By implementing these recommendations, the government can take substantial steps towards building a more inclusive and equitable healthcare system that benefits all citizens of Pakistan.
Introduction
Pakistan faces profound healthcare disparities, leading to unequal health outcomes across various demographics. In Pakistan, there are two separate healthcare systems – one is run by the government (public hospitals), and the other is private hospitals. The public hospitals lack even basic healthcare facilities, while the private ones are too expensive for most people in Pakistan to afford. To improve the healthcare system in Pakistan, two important things are needed: enough money to support the system and the infrastructure development of better facilities and services. Without these investments, the healthcare system will keep struggling to survive and won’t be able to compete with other countries in the region.
Healthcare disparities in Pakistan represent a multifaceted and pressing challenge that continues to hinder the nation’s progress towards achieving equitable access to quality healthcare for all its citizens. Despite significant efforts to improve healthcare infrastructure and services, Pakistan grapples with persistent inequalities in health outcomes, access to medical facilities, and affordability of healthcare, particularly among vulnerable and marginalized populations. These disparities are deeply entrenched and influenced by a complex interplay of socio-economic, geographic, cultural, and gender-related factors, exacerbating the gap between the health status of different population groups.
Pakistan, as a populous and diverse nation, is home to over 220 million people, residing in both urban centers and remote rural areas. The distribution of healthcare facilities is heavily skewed, with major urban centers enjoying better healthcare infrastructure, access to specialized medical services, and highly skilled healthcare professionals. However, the majority of the country’s population resides in rural and underserved regions, where access to healthcare remains a significant challenge. As a result, these regions face higher mortality rates and morbidity rates due to preventable diseases and inadequate medical interventions.
Socioeconomic status is a crucial determinant of healthcare disparities in Pakistan. A considerable portion of the population lives below the poverty line, struggling to meet basic needs, including healthcare expenses. The burden of out-of-pocket healthcare costs disproportionately affects the poor, often leading them to forgo medical treatments or seek substandard care. The consequences of this financial strain are severe, contributing to a cycle of poverty and poor health outcomes.
Furthermore, healthcare disparities are intricately linked to gender inequalities in Pakistan. Women, especially in rural areas, encounter significant barriers to accessing healthcare, often due to cultural norms, lack of autonomy, and restricted mobility. As a result, maternal and infant mortality rates remain alarmingly high, with many women unable to access essential maternal care during pregnancy and childbirth.
Healthcare disparities also intersect with education and health literacy. Many individuals lack knowledge about preventive health measures, leading to delayed medical interventions and increased disease burden. Low health literacy is a significant challenge in implementing effective health education campaigns and promoting behavior change for better health practices.
Infectious diseases continue to pose significant threats to public health in Pakistan. Outbreaks of diseases like malaria, tuberculosis, and polio disproportionately affect vulnerable populations, particularly those living in overcrowded urban slums and remote rural areas. These outbreaks are exacerbated by weak healthcare infrastructure, inadequate vaccination coverage, and limited access to clean water and sanitation facilities.
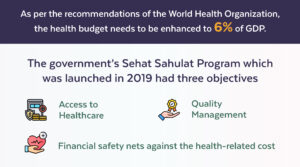
While the Pakistani government has undertaken various initiatives to address healthcare disparities, including the launch of the National Health Vision 2025, substantial challenges persist in translating policies into actionable improvements on the ground. Insufficient funding, mismanagement, corruption, and fragmented healthcare delivery systems have hindered the effective implementation of health initiatives.
As the nation confronts these formidable healthcare challenges, it is essential to emphasize the urgent need for innovative and evidence-based solutions. Policymakers, healthcare professionals, civil society organizations, and the private sector must work collaboratively to develop a comprehensive approach that tackles healthcare disparities from multiple angles.
This policy brief aims to delve deeper into the root causes of healthcare disparities in Pakistan, explore the specific challenges faced in addressing them, and present a range of innovative and effective recommendations to bridge the gap. By adopting a holistic and equitable approach to healthcare, Pakistan can move towards a future where all citizens have access to quality medical services, irrespective of their socioeconomic status, geographic location, or gender. By embracing inclusivity and social justice, the nation can pave the way for improved health outcomes, increased productivity, and a more prosperous and healthier society.

Policy Recommendations
Some of the reasons for healthcare disparities are uneven access to facilities, shortage of health case professionals, lack of health insurance, maternal and child health, low health literacy and insufficient funding. Below are some of the recommendations with their challenges that are faced in Pakistan:
Identifying Disparities
Healthcare disparities in Pakistan arise from various factors, including geographical location, socioeconomic status, gender, and cultural norms. Such services in Pakistan are disproportionately concentrated in urban areas, leaving rural and remote regions with limited access to quality medical facilities. Urban-rural gaps persist due to uneven distribution of healthcare facilities, with urban areas benefiting from better infrastructure and skilled healthcare professionals. Socioeconomically disadvantaged populations often struggle to afford essential medical services, leading to suboptimal health outcomes.
Challenges
– Limited healthcare infrastructure in remote and underserved regions.
– Uneven distribution of healthcare professionals, with urban areas attracting most skilled practitioners.
– Inadequate funding for healthcare, particularly in rural areas.
– Low health literacy and awareness, hindering preventive healthcare practices.
Enhancing Healthcare Infrastructure
Recommendations
– Prioritize investment in healthcare infrastructure in rural and underserved areas to expand access to medical facilities.
– Develop telemedicine services to reach remote populations, offering consultations and monitoring services remotely.
– Implement health facility mapping to identify areas with the greatest need for healthcare facilities.
Challenges
– Limited funding and resources for infrastructure development in remote regions.
– Attracting healthcare professionals to work in challenging rural environments.
Strengthening Primary Healthcare
Recommendations
– Enhance the primary healthcare system by equipping facilities with skilled healthcare professionals, essential medications, and medical equipment.
– Promote a community-based approach to healthcare, integrating local healthcare workers and traditional practitioners into the system.
– Implement a comprehensive vaccination program to prevent communicable diseases and improve public health.
Challenges
– Shortage of qualified healthcare professionals in primary care settings.
– Inadequate training and resources for community healthcare workers.
Investing in Human Resources
Recommendations
– Establish incentives for medical graduates to work in underserved areas, such as financial incentives, scholarships, and mandatory rural service programs.
– Strengthen medical training programs, especially for primary care providers, to improve their skills and competencies.
– Foster collaboration with medical schools to create awareness about the significance of serving in underserved regions.
Challenges
– Attracting healthcare professionals to rural and remote areas.
– Sustaining healthcare workforce retention in challenging environments.
Expanding Health Insurance Coverage
Recommendations
– Work towards universal health coverage to ensure all citizens have access to essential healthcare services.
– Establish public-private partnerships to make health insurance more affordable and accessible to vulnerable populations.
– Implement targeted subsidy programs for low-income individuals to ensure they can afford health insurance.
Challenges
– Insufficient funding for universal health coverage programs.
– Limited awareness about health insurance and its benefits among marginalized communities.
Promoting Health Education and Awareness
Recommendations
– Launch health awareness campaigns, tailored to the cultural and linguistic diversity of the population, to promote preventive healthcare practices.
– Invest in health education programs in schools and communities to improve health literacy.
– Use digital platforms and community engagement to disseminate health information effectively.
Challenges
– Overcoming cultural barriers and beliefs that may hinder adopting preventive healthcare measures.
– Reaching remote populations with limited access to media and information channels.
Collaboration with NGOs and Private Sector
Recommendations
– Encourage collaboration between the government, NGOs, and private sector to optimize healthcare resources and reach underserved populations.
– Create a framework for public-private partnerships to ensure transparent and ethical cooperation.
– Facilitate private sector investment in healthcare infrastructure and services in underserved areas.
Challenges
– Ensuring equitable distribution of resources and services through collaborations.
– Maintaining accountability and quality standards in private sector involvement.
Monitoring and Evaluation
Recommendations
– Establish a robust monitoring and evaluation system to assess the impact of healthcare interventions and identify areas for improvement.
– Use data-driven decision-making to optimize resource allocation and policy implementation.
– Involve stakeholders in the evaluation process to ensure inclusivity and transparency.
Challenges
– Limited data availability and accuracy in some regions.
– Building capacity for data collection and analysis in healthcare systems.
Conclusion
The healthcare disparities in Pakistan present a sobering reality, highlighting the urgent need for comprehensive and targeted measures to create a more equitable and inclusive healthcare system. As the country grapples with the challenges of unequal access, inadequate resources, and gender disparities, addressing these issues has become an imperative for sustainable development and better health outcomes for all citizens.To bridge the gap between the healthcare services available in urban and rural areas, there must be a concerted effort to enhance healthcare infrastructure in underserved regions. Investments in building and upgrading medical facilities, equipping them with essential medical equipment, and recruiting skilled healthcare professionals to serve in remote areas are crucial steps in achieving this goal.
Improving maternal and child health is paramount in reducing mortality rates. Ensuring access to skilled maternal care during pregnancy and childbirth, coupled with effective immunization programs and nutrition initiatives, can significantly contribute to better health outcomes for mothers and children.
To address infectious diseases, it is essential to strengthen disease surveillance, vaccination programs, and disease prevention strategies. Targeted interventions aimed at vulnerable populations can help curb outbreaks and reduce the disease burden.Moreover, the healthcare system can benefit significantly from expanding health insurance coverage, particularly for low-income and marginalized communities. Universal health coverage can relieve the financial burden on families and increase access to essential medical services.
Addressing gender disparities in healthcare necessitates fostering an environment that promotes gender equality and women’s empowerment. Enabling women to make informed decisions about their health and well-being is crucial to improving overall health outcomes in Pakistan. Promoting health literacy through educational campaigns and community engagement is vital to empowering individuals to take charge of their health. Raising awareness about preventive health practices can lead to healthier lifestyle choices and reduced disease prevalence.
A critical aspect of combating healthcare disparities in Pakistan involves boosting funding and financial support for the healthcare sector. Adequate allocation of resources is vital for improving medical facilities, healthcare services, and research and development. Furthermore, addressing mental health challenges must be a priority. Removing the stigma surrounding mental health and enhancing access to mental healthcare services will significantly improve the overall well-being of the population.
In conclusion, bridging healthcare disparities in Pakistan requires a collective effort from policymakers, healthcare providers, civil society organizations, and the private sector. A comprehensive approach that emphasizes equitable access, healthcare infrastructure development, health education, and gender equality is essential to achieving improved health outcomes for all citizens. By investing in the healthcare system, Pakistan can lay the foundation for a healthier, more prosperous future, and ensure that its healthcare system competes with the best in the region, ultimately leading to the well-being and prosperity of the entire nation.
References
https://assets.cureus.com/uploads/editorial/pdf/161591/20230710-4592-1yspsm3.pdf
https://sdpi.org/analyzing-health-budget-2023-in-context-of-wellbeing-of-people/news_detail
file:///C:/Users/momina/Downloads/ccsbrief_pak_en.pdf
https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-023-00904-1



Leave a Reply